Before the Shovel Hits the Ground Part 2: Key Considerations for Developing a New Hospital or Major Capital Investments - Design & Pre-Construction Phase
By Aimee Alix Fogarty, Regional Vice President, Hammes Healthcare
Building off Hammes’ “Before the Shovel Hits the Ground” article where we explored the strategy, site, approvals, and team selection phase of a project, we now turn our focus to the next phase of design and preconstruction. Once there is a strategy in place, a financing source identified, land selected, and a space program approved, the complicated process of design development and documentation can start. At this stage, depending on project size, the team of consultants can grow to over 50 professionals who are each focused on a task that requires specific knowledge that cannot be completed in a silo. Establishing a functional and efficient team structure and safeguarding healthy team communication is imperative to project success.
Key elements to consider at this stage of the project include:
- Team Organization & Key Stakeholders to Support Decision Making
- In-House Health System Department Readiness
- Legal
- Procurement & Accounting
- Financial Management
- Communications
- Total Project Scope, Budget, & Schedule
- Decision Making
1. Team Organization & Key Stakeholders to Support Decision Making
As the team structure forms, the process and timeline to make certain decisions will form too. You will need to create a group of leaders, typically called a steering committee or executive leadership group, to provide final direction on questions that arise along the way. This may include unforeseen conditions, new requirements not accounted for previously, or user group requests for changes. Your project management team can help create a template on information needed from the team such as cost, schedule or operations impact for each item, so decision making is streamlined. Your management team can also work with you to decide what decision items need to be escalated to leadership and which ones can be resolved at the project level.
On large, complex healthcare projects, there are internal and external stakeholders. It is important to identify these stakeholders at the beginning of the project to ensure each understands their role and responsibility on the project.
At the highest level, from the health system board to the steering committee, the project team must be kept current on the status of the project. The project management team can help create the structure of the report and/or presentation, frequency of the meetings, and process for pulling that information together on a regular basis with key messaging for the board.
A good project management practice is to create a project charter that will serve as the governance document. This charter will typically identify groups who will participate and their role and responsibility. Important groups on a project team include the Owner/user groups, planner/programmer, architect, engineers, and construction manager, as well as various consulting groups and their sub-specialties. Some consultants may directly work with your in-house team members and hold agreements with your system. These groups normally have a key leading role on the project or manage sensitive information. The structure of the team is important as it dictates flow of information, funds, and risk.
In beginning with the end in mind, it is also important to consider the activation of the new facility and your team that will be providing patient care within it. It is recommended that your project team include an operational readiness expert during the design of the project so there is a clinical and operational voice at the table from the start. Why is this important? “Building readiness” and “patient readiness” are not the same. Operational readiness develops and manages an informed operational work plan to identify and coordinate activation activities and departmental tasks such as staffing and training, revenue cycle and billing, regulatory and accreditation, emergency preparedness, operational practice and contract and licensure tracking.
2. In-House Health System Department Readiness
a. Legal
The Owner of the project (usually the health system or the funding entity) needs to protect their investment. Contracts are designed to protect your interest when unforeseen conditions may impose a risk to the project. In addition, parties in your project team will rightfully seek to include verbiage in their contracts to limit their respective risks, responsibilities, and liabilities.
There are various organizational structures under which the construction team, design team, and the Owner interact (i.e., Integrated Project Delivery, Design-Bid-Build, Design-Build, Guaranteed Maximum Price). Each structure may require a different contract to ensure all parties assume some level of financial responsibility for the success of the project. Your in-house legal department (or outsourced, if needed) must be ready to undertake the legal review and approval for each of the contracts in a timely manner so the project is not impacted.
b. Procurement & Accounting
The Owner is responsible for securing funding for the project, and ensuring all parties are paid in a timely manner. Once contracts are signed, the health system’s procurement department is responsible for issuing the relevant purchase orders (POs). Depending on the size of this department and project, this can be overwhelming. A seamless process and communication structure is important to maintain project momentum and cash flow.
Once POs are issued, invoices can commence. Payments that are part of routine project activities are usually made after receipt of each invoice. Your project management team will be instrumental in ensuring that the amount billed corresponds with job progress and stays within the established budget. They can also communicate with the procurement and accounting teams on the timing of POs and invoicing through the overall project scheduling, draw, and forecasting process. This is a critical communication stream given the current supply chain environment. At the end of a project, all POs will need to be reconciled and closed out. Therefore, it is important this process is established and adhered to from the very beginning of the project.
c. Financial Management
A strong setup for project financial management and project controls during design and preconstruction is the foundation of a successful project. Some may think nothing happens until construction, but that couldn’t be further from the truth! Key aspects to consider include budgeting, cost estimation and tracking, budget control reports, risk management, contracts, cash flow management, contingency planning, cost-benefit analysis for design options, and compliance/reporting for all sources and uses of a capital stack. By prioritizing cost control and budget management throughout the lifecycle of a major healthcare capital project, stakeholders can mitigate financial risks, optimize resource allocation, and ensure the project's financial success and sustainability.
d. Communications
Communication is a central vein of a successful project! For large, complex projects with many stakeholders, it is imperative that all communications are synchronized, timely, and accessible. A critical tool is a communications plan, approved by the Owner, to define the process and points of contact required for approval before formal communications go out. Important components of this communications plan include a stakeholder assessment, communications gap analysis, goals and objectives, key messaging, schedule and milestones, feedback mechanisms, crisis management, and budget recommendations. Communication can come in the form of news releases, websites, apps, and social media. Messaging on all platforms should be consistent, positive, and get the community excited for the new project.
By systematically addressing these components in a communications plan for a new hospital project, project leaders can foster positive stakeholder relationships, enhance project transparency, and support successful project outcomes. A strong communications consultant can provide support in this effort.
3. Total Project Scope, Budget, & Schedule
Prior to selecting the architectural, engineering, construction, and/or consultants, the project scope, budget, and schedule parameters should be set. This is important as they are key drivers in the contract basis. The Owner must communicate their system strategic plan and related business plan (in the form of key planning units (KPUs) for the new facility so scoping, programming and blocking/stacking can begin.
In parallel, a conceptual budget plays a crucial role in guiding design teams on a capital project by providing a framework within which they can develop design solutions that align with financial constraints and project goals. This conceptual total project budget should contain basic components such as hard costs (sitework, construction, equipment), soft costs (consultants, escalation, phasing, AHJ requirements, insurances), medical equipment, furniture, art, signage, capitalized interest, escalation, and Owner contingencies. It is helpful to evaluate key metrics like cost-per-bed and/or cost-per square-foot for benchmarking purposes. By setting the total project budget at the onset of the project, you are setting financial parameters, encouraging cost-conscious design, and facilitating stakeholder alignment. You are also setting the overall target for the design and construction team who will breakdown the design packages and assign a ‘target value design’(TVD) to each, totaling the overall target. Any design options that are presented and discussed, must run the TVD gauntlet as part of the decision-making process for the project, as discussed in the next section. The design team is ultimately responsible for designing to the set budget, which should avoid rework and value engineering in later project phases.
Why is it important to understand the total project budget? There are other considerations outside of design and construction. For example, some current healthcare spending trends that could detract from the capital dollar budget “pie” include:
- Technology integration (electronic health records, telemedicine platforms, AI-driven diagnostics, and IoT devices)
- Sustainability initiatives (as more organizations are investing in more eco-friendly and energy efficient buildings)
- Adaptation to regulatory changes (upgrades to comply with safety standards, cybersecurity measures, or changes in reimbursement models)
- Overall compression in financial spend (including prioritization of projects based on ROI and seeking other funding sources)
Lastly, during design and preconstruction, the project schedule is vital as it supports effective coordination, time management, budget control, risk management, stakeholder engagement, decision-making, compliance with contractual obligations, quality assurance, and overall project efficiency. It serves as a roadmap for achieving project milestones and delivering successful outcomes within the planned timeframe. It should contain milestones like completion of key design phases, grant or other interim financial milestones, GMP package completion, early release equipment, permits, construction start, construction substantial completion, transition/activation, and go-live/first patient day.
4. Decision Making
As we are specifically talking about design and preconstruction, decision-making during this phase of a major healthcare capital project is crucial because of its significant impact on project success, cost management, functionality, and stakeholder satisfaction. As shown in the image below, decisions made early in the process have the greatest impact on the overall project. However, the spending and cash flow related to project occurs much later.
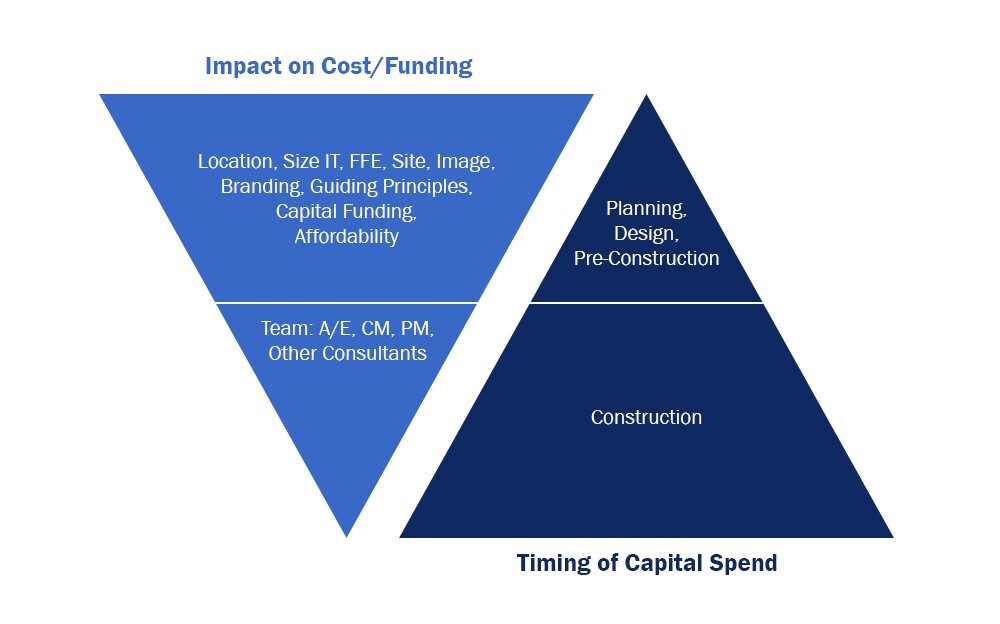
Effective decision-making during the design and preconstruction phase influences key aspects of the project, including impact on patient care and safety, cost, regulatory compliance, integration of technology, flexibility and future expansion, sustainability, and engagement of stakeholders. Your project management team will be required to have a comprehensive understanding of clinical, operational, financial, regulatory, technological, and environmental factors, and organize and arm you, the Owner, with the information needed to drive timely decisions throughout the course of the project. By making informed decisions that balance these considerations, healthcare organizations can create facilities that support optimal patient care, operational efficiency, sustainability, and stakeholder satisfaction throughout the project lifecycle.
Once a project has a strong foundation in the design and preconstruction phase, construction and execution of the plan can commence. After that, you move into the final phase of capital project development—project execution—i.e. after the shovel hits the ground!
Aimee is a Regional Vice President with Hammes Healthcare. Over the past 21 years, Aimee has been involved in the planning, design, and construction of more than $10 billion in healthcare projects, delivering successful outcomes for clients on major capital programs. Aimee has extensive experience and relationships in the construction industry, having worked with large construction management firms before joining Hammes. Aimee holds a Master of Real Estate Development (MERD) and has held her Certified Healthcare Constructor (CHC) certification since 2008.